Hello everyone,
Death it’s a topic that no one wants to talk about. Very morbid, very uncomfortable, very sad. However, it’s the inevitable for all us humans. Let’s talk about it.
If your first instinct reading the first paragraph was to stop reading, pause, and feel the uncomfortable. Happiness, progress and peace sits beyond our ability to face these feelings, not run away from them. In this article we will discuss the risk of 31 disease and answer the big question:
Does having PCOS affect how long we can live?
I debated weather I should make this a paid post. A lot of work and thought went into writing it and ensuring I present you with the right facts. However I think it’s such key information for all of you that I decided to keep it free. If you take value from my writing, I would appreciate if you’d upgrade to paid so I can continue bringing you high quality information about PCOS.
I am part of a book club and January’s book was With the End of Mind by Kathryn Mannix, a palliative care doctor. The book goes through stories of people dying and the aim with her writing is to make people feel more comfortable with the thought of dying. The premise is that we made death clinical and dramatised through TV and soap operas. The process of dying was once something that we all withnessed but with the advancement of medicine we go through life not having seen someone dying. However she goes on to describe dying as she has experiences countless time in her career as peaceful, non-violent and natural.
Unfortunately, I have already read my fair share of death books when my dad passed away. It was my first encounter with unexpected death. I had lost my grandmother before that but it was somehow expected. My dad was 50’s when he lost his life. At that time I found peace in reading stories of people who have gone through cancer diagnosis, spirituality and living through having a terminal diagnosis. At that time, I found them comforting as if I was sharing the pain with someone.
This time around, reading this book was hard. It was challenging because I was now thinking of my own mortality and not my dad’s. If you chose to read it prepare for crying. Not a book you can read on public transport. A book that is uncomfortable but somehow needed to dismantle the taboo of death.
This introspection made me think about our condition and how it impacts our longevity. We hear about all of the different diseases we have a risk for, but does having PCOS affect how long we can leave?
I will tell you know that this research was hard to conduct. It’s very uncomfortable to think about your own trajectory. However it does help to understand why we must take care of our health and why our efforts in staying healthy are important.
Let’s do some deep dive into the research.
I looked into 5 different studies and there are some good news, some bad news and some conflicting news.
The bad news
If you are a half glass full person, maybe start with the good news.
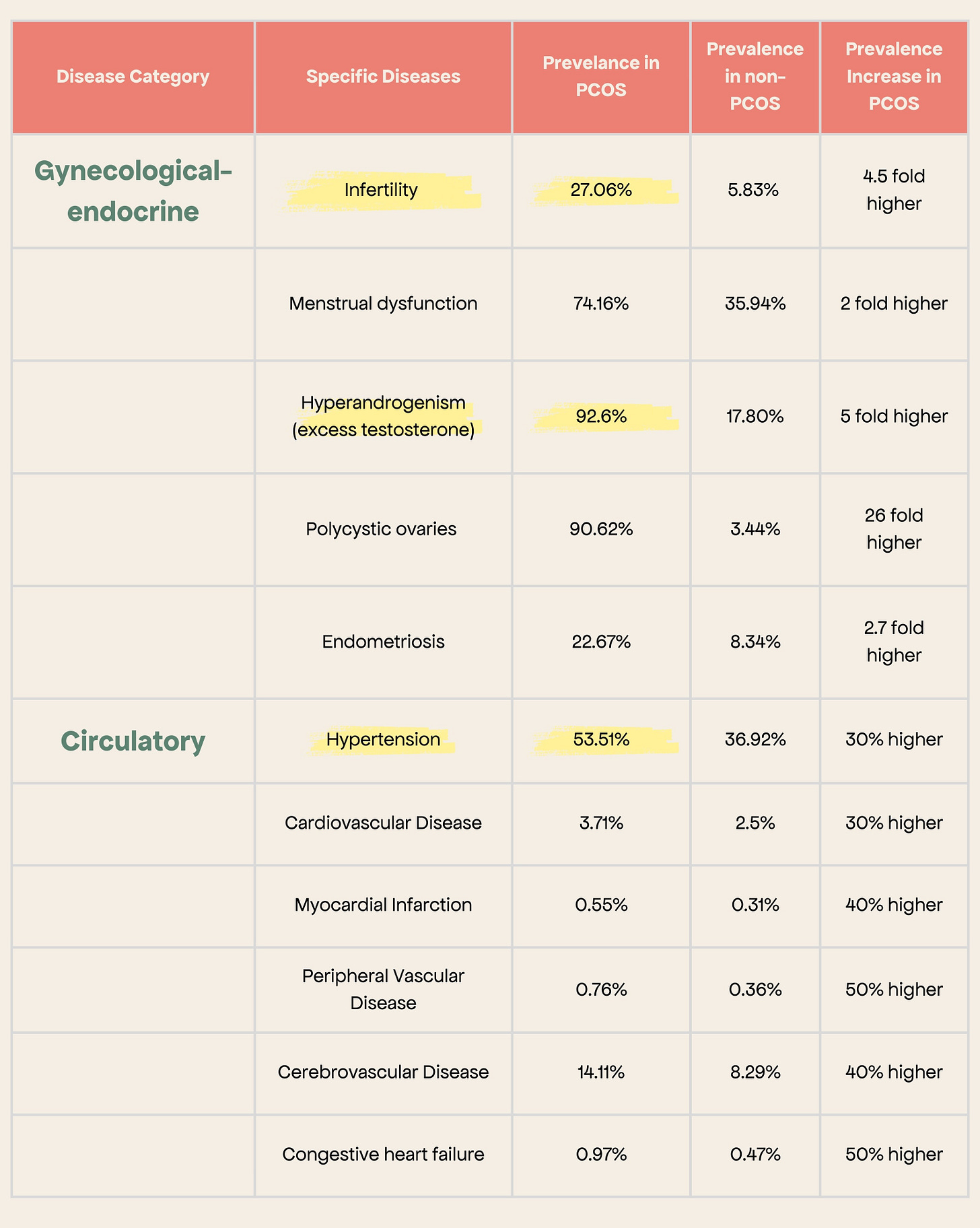
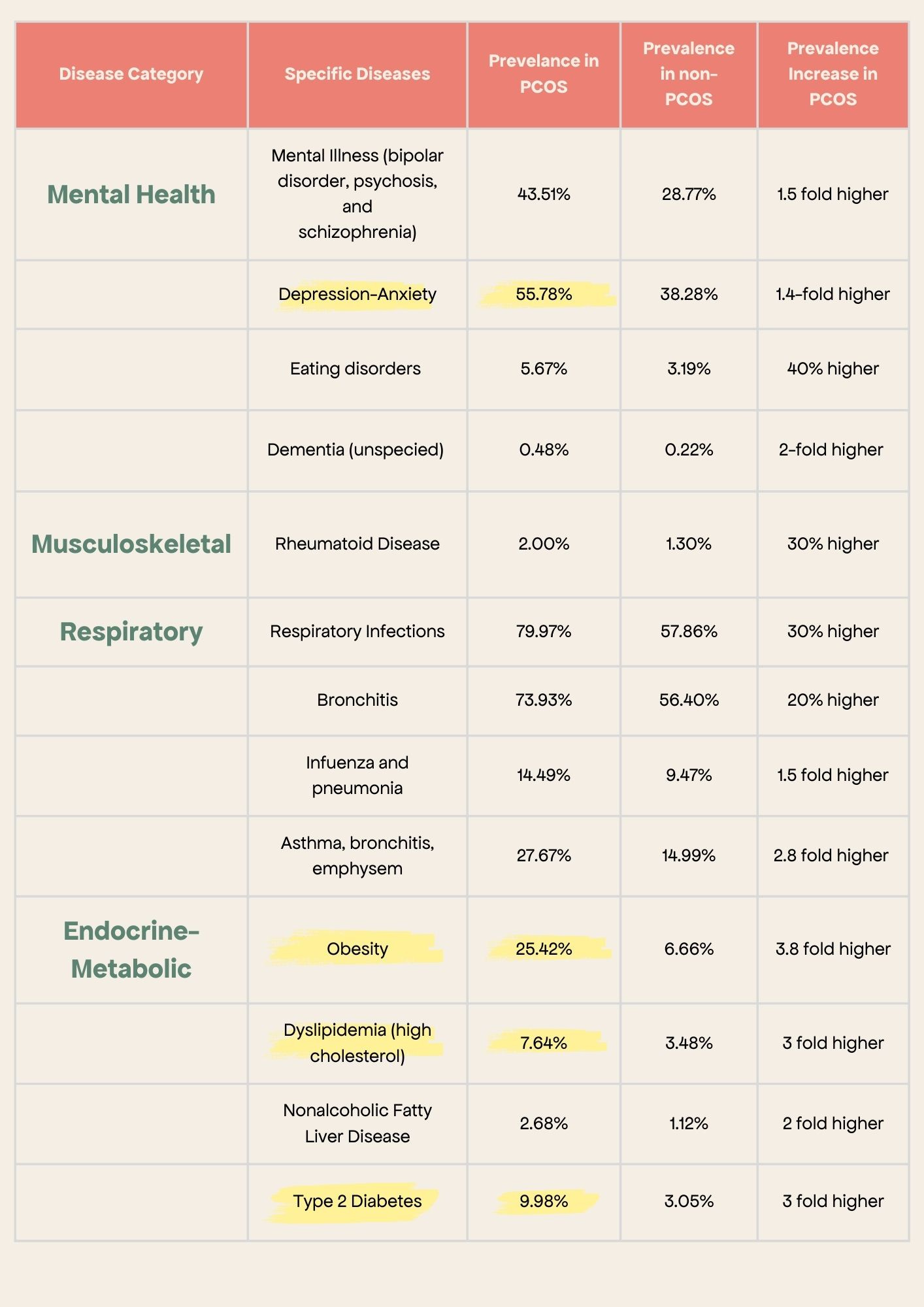
The bad news is that we have an increased risk of every disease under the sun (yay to us). This is a table from a study done from 2002-2018 in Alberta, Canada. It includes data from 16,531 PCOS cases and 49,335 age-matched non-PCOS cases (you might want to open this one on a computer).
It is important to note that a 50% increase in risk is considerable but the prevalence if super important. For example, for Myocardial infraction (heart attack) our risk is 40% higher but it happens in about 0.55% of PCOS cases. Compared to infertility for which we have 4.5 fold higher risk and it happens in 27.03% of cases.
I highlighted in yellow the ones that I think we need to pay attention to throughout our early life so we don’t suffer in our later life.
As a result of the above there are some big areas we must work hard to lower the risk:
Infertility - we will explore this topic in depth this year through numerous articles
Excess testosterone - this affects all others including obesity, high cholesterol, endometrial cancer
Depression and Anxiety - extremely important to look after our mental health considering also the risk of more serious mental illnesses
Obesity - we know this by now and I don’t think I need to repeat it
Type 2 diabetes - this is one that goes hand in hand with obesity and insulin resistance.
High Cholesterol - testing and keeping an eye on this marker is extremely important for us
Endometrial Cancer - I will write an in-depth article about this one soon
Gastro intestinal - looking after our digestive system it’s super important because these disease are quite painful and will also affect our mental health. As a result this becomes even more important
If you look at this list,
We have some power over it.
Some of these diseases are preventable with the right lifestyle which is eating whole food focused on nutrient density, eating enough fibre, working out and finding space to relax and decompress. Looking after your PCOS is not an option, it’s a mandatory action if we want quality of life as we age.
Please note that this study was done based on medical codes. This means that they were inputted in a consultation with a healthcare professional so by default everyone had something. They did no look at PCOS women who have never come to a doctor’s office with a complain. In addition it doesn’t take in consideration lifestyle or dietary habits. I would treat the number with caution but take the lesson. The increased risk of disease for PCOS women has been replicated in numerous studies so it definetely exists.
Ok, but we still have the question of does having PCOS affect how long we can live? Let’s go into some good news.
The good news
A study published in 2023 followed a well-defined cohort of women diagnosed with PCOS, along with an age-matched reference group, for 32 years.
Some key findings:
No increase in all-cause mortality or CVD-related mortality was found in women with PCOS compared to the reference group, even at a mean age of 81 years.
While women with PCOS showed a higher prevalence of CVD risk factors like hypertension and elevated triglycerides in earlier follow-ups (at perimenopausal age and mean age 71), these differences disappeared by the time they reached a mean age of 81.
The only significant difference observed at baseline (32 years prior) between deceased and living women with PCOS was a higher waist-hip ratio (WHR) in the deceased group.This suggests that abdominal fat distribution might be a more critical factor in long-term health outcomes than previously thought.
This is a bit confusing. We have higher risk of disease but doesn’t seem like it leads to us dying younger. The authors of this study proposed a few explanations of why:
The remaining higher testosterone levels in postmenopausal women with PCOS might have a protective effect, counteracting other CVD risk factors. We looked into what happens to women in Menopause in the article below.
The wedge resection surgery (no longer performed for us) that all the women with PCOS in this study underwent might have contributed to a reduction in PCOS symptoms and obesity, particularly abdominal obesity. However, the study does not definitively confirm whether the surgery itself is protective or not.
The conflicting news
3 other studies showed an increase in CVD risk for women with PCOS. The issue is that they don’t mention mortality but focus on incidence.
However there is one abstract that is receiving a lot of attention from publications who showed a significantly higher mortality rate in women with PCOS. I am unable to find the whole study so I am only reporting on very little data on this study. I have emailed the journal for the full study.
The researchers used ICD codes to identify 9,839 women with PCOS and matched them with 70,705 controls based on birth year and residential area from the Finnish Care Register for Health Care from 1969 to 2019. They then tracked mortality and causes of death. They found:
Women with PCOS still had a 47% higher risk of dying during the study period compared to women without PCOS
Some of the main causes:
Diabetes - a 207% higher risk of dying from diabetes compared to women without PCOS.
Other circulatory system diseases - 107% higher risk of dying from other circulatory system diseases compared to women without PCOS.
Bronchitis - 261% higher risk of dying from bronchitis compared to women without PCOS.
Tumors - 38% higher risk of dying from tumours compared to women without PCOS.
The sadder part of this finding is that women with PCOS died younger than the control group (average age 51.4 years vs. 52.9 years).
It’s important to note that the numbers of deaths were were 177 deaths/ 9839 for women with PCOS and 1,003/70,705. The sample size it’s small.
We know there's a higher risk, but we don't know how many people actually died. The study doesn't tell us the incidence rates, which means we don't know how common these deaths actually were in both groups. It's like knowing it's more likely to rain tomorrow but not having a percentage chance.
We don't know how long the researchers followed each person in the study. They collected data from 1969 to 2019, but people could have entered the study at any time. This makes it hard to compare the death rates accurately. Imagine comparing the number of car accidents on a busy road for a whole year versus just for one hour – it wouldn't be a fair comparison.
Whilst this study might provoke a strong emotion, please bear in mind these are risk increases. It’s not an absolute terms that we will die at 50’s.
Closing thoughts
To conclude, yes, PCOS can affect how long we can live. Some of it will be in our control, some of it not quite. However, there is a powerful thing I am taking from writing this article and facing it: looking after ourselves is not negotiable. We can lead with emotions: it’s not fair, it’s annoying, it’s sad. Whilst we should allow ourselves to feel these emotions, our response is more important to it. I want to live till my old age, kicking and enjoying the outdoors. This is why I invest in my health money, time and effort. I know it will pay off. My worst case scenario would be looking back and saying I could have done more. I think you can have a long
I hope this didn’t make you too sad.
See you next Sunday,
Francesca
Berni, T. R., Morgan, C. L., & Rees, D. A. (2021). Women with polycystic ovary syndrome have an increased risk of major cardiovascular events: A population study. The Journal of Clinical Endocrinology and Metabolism, 106(9), e3369–e3380. https://doi.org/10.1210/clinem/dgab392
de Groot, P. C. M., Dekkers, O. M., Romijn, J. A., Dieben, S. W. M., & Helmerhorst, F. M. (2011). PCOS, coronary heart disease, stroke and the influence of obesity: a systematic review and meta-analysis. Human Reproduction Update, 17(4), 495–500. https://doi.org/10.1093/humupd/dmr001
Forslund, M., Schmidt, J., Brännström, M., Landin-Wilhelmsen, K., & Dahlgren, E. (2022). Morbidity and mortality in PCOS: A prospective follow-up up to a mean age above 80 years. European Journal of Obstetrics, Gynecology, and Reproductive Biology, 271, 195–203. https://doi.org/10.1016/j.ejogrb.2022.02.020
Glintborg, D., Rubin, K. H., Nybo, M., Abrahamsen, B., & Andersen, M. S. (2018). Cardiovascular disease in a nationwide population of Danish women with polycystic ovary syndrome. Endocrine Abstracts. https://doi.org/10.1530/endoabs.56.gp127
Pierpoint, T., McKeigue, P. M., Isaacs, A. J., Wild, S. H., & Jacobs, H. S. (1998). Mortality of women with polycystic ovary syndrome at long-term follow-up. Journal of Clinical Epidemiology, 51(7), 581–586. https://doi.org/10.1016/s0895-4356(98)00035-3
Polycystic Ovary Syndrome Is Associated With an Increased Mortality Risk. (n.d.). R35-36.
Vine, D., Ghosh, M., Wang, T., & Bakal, J. (2024). Increased prevalence of adverse health outcomes across the lifespan in those affected by polycystic ovary syndrome: A Canadian population cohort. CJC Open, 6(2Part B), 314–326. https://doi.org/10.1016/j.cjco.2023.12.010
Disclaimer: We are all unique in our ways, so this information is for educational purposes only. In my communications, I summarise research data and bring my experience. This shouldn’t be viewed as medical advice at any point. Please consult your healthcare provider further about your health needs.