Hello everyone,
Today I am bringing you Episode 2 of our Feritily series. As a reminder this is a five part series to deep dive into our ability to conceive with my colleague Daria, a Nutritional Therapist who specialises in fertility.
PS: the articles are both in video and written format to fit both preferences of consuming information.
We discuss how to prepare your body for pregnancy using Daria’s four pillars:
Exclusive for members: This in-depth article is part of our premium content. Subscribers enjoy comprehensive PCOS deep-dives, customised meal plans, expert medical insights, and direct access to ask me questions. Invest just £1.74/week in understanding and managing your PCOS effectively.
Where should I start?
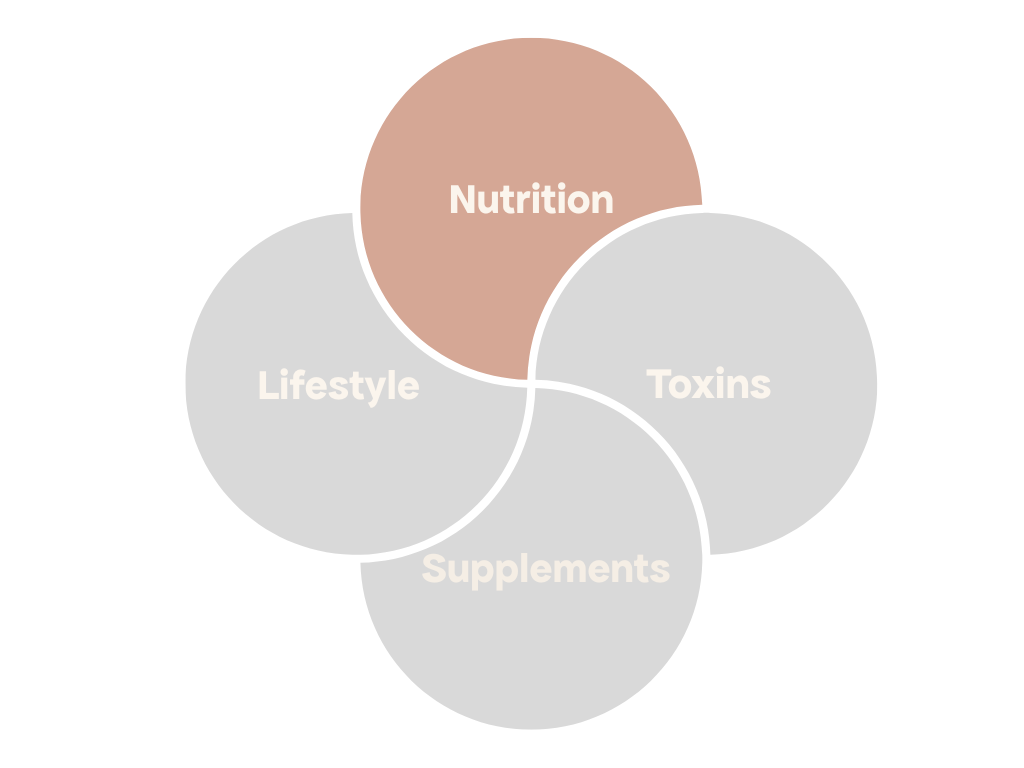
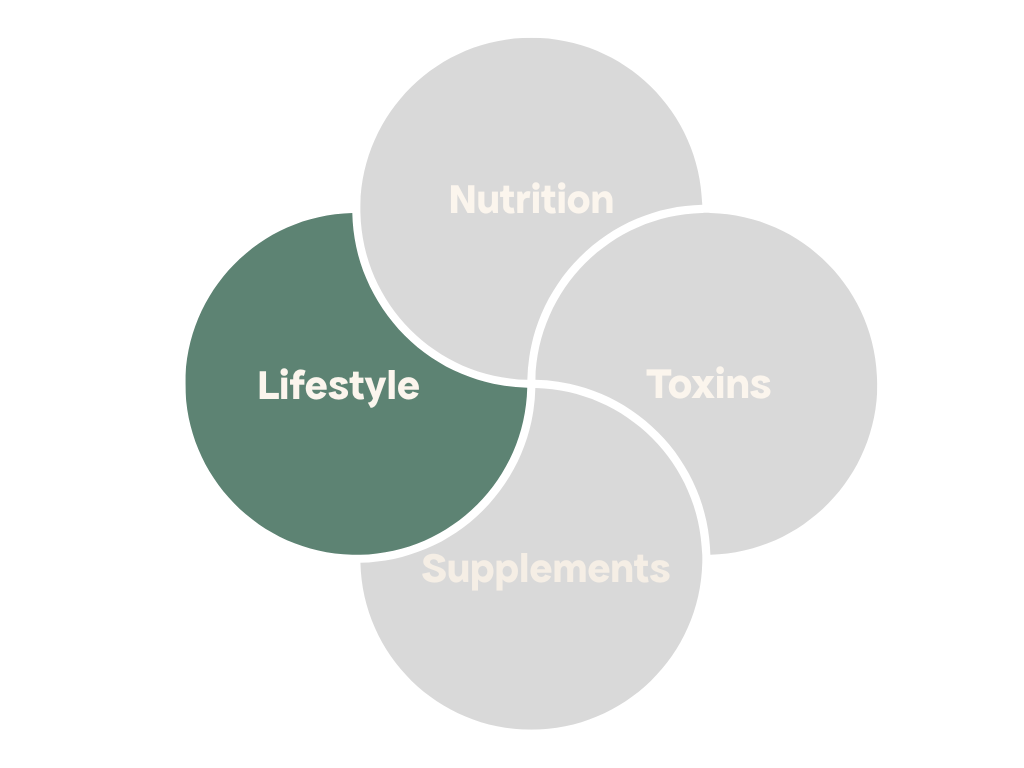
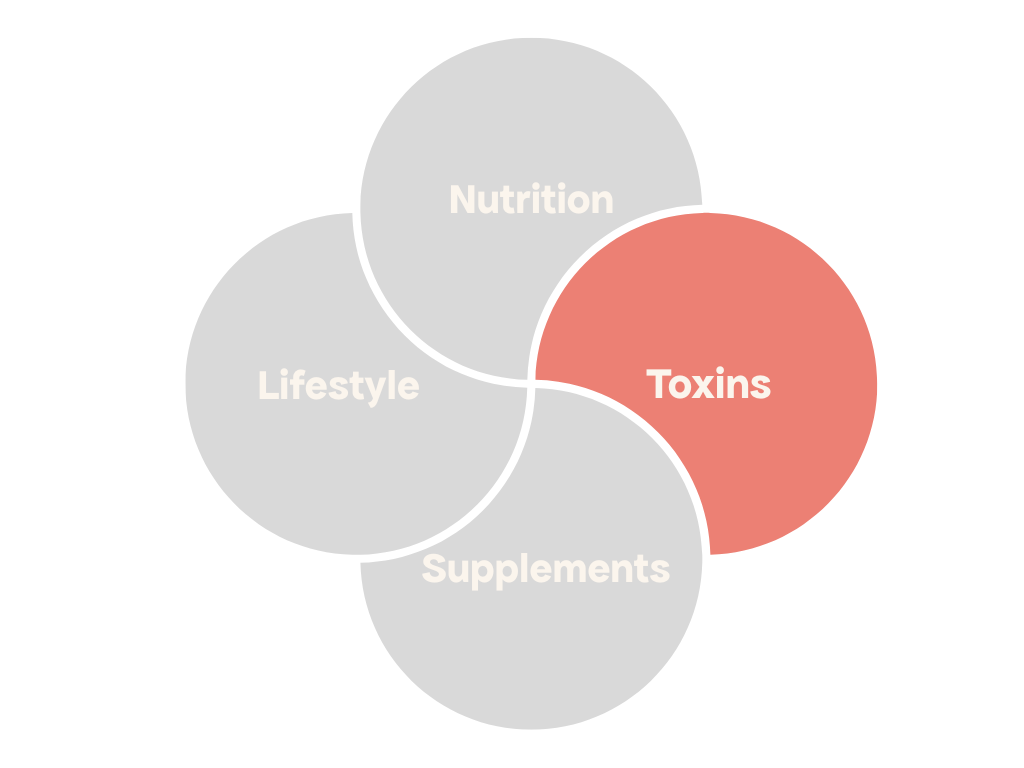
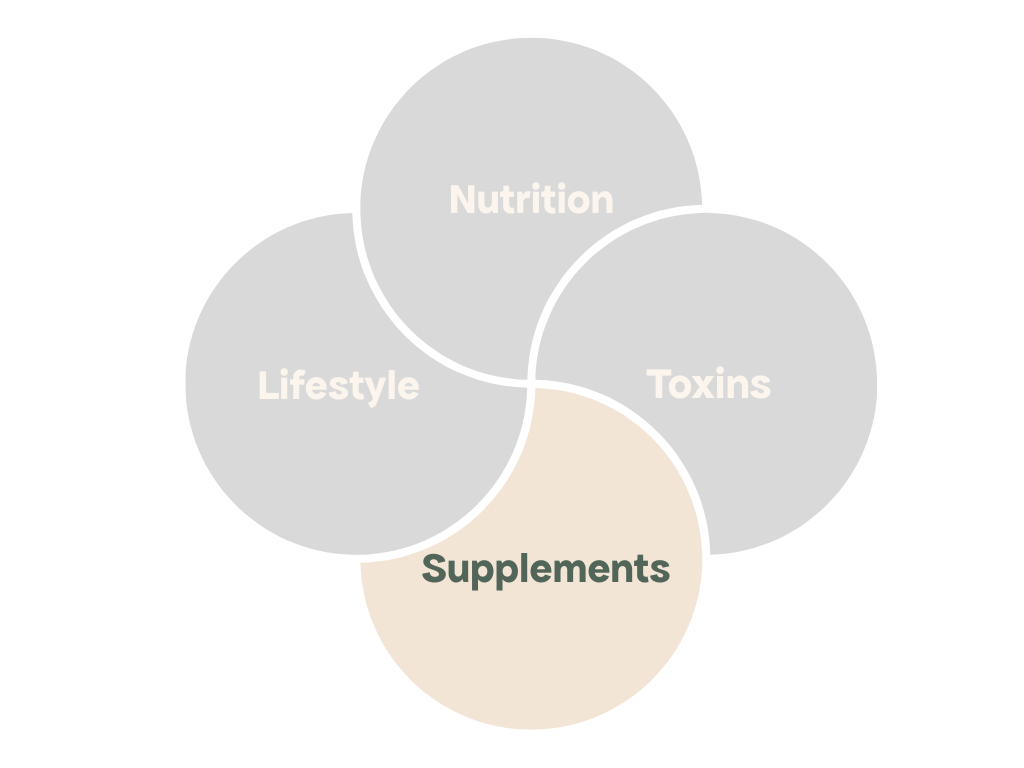
When preparing for pregnancy with PCOS, adopting a mindset focused on long-term health for yourself and your future baby can make a significant difference. Instead of approaching this as a short-term effort, think of it as creating a foundation of health that benefits you and your family for years to come. This journey isn’t just about conception but about nurturing your body to thrive. PCOS can present unique challenges, but with the right approach, you can create a supportive environment for conception. In this article, we will discuss a realistic timeline for preparation and focus on four key pillars: nutrition, lifestyle, toxicity management, and supplements.
Start thinking of yourself as pre-pregnant
Your preparation for pregnancy begins well before conception. The cell that becomes your egg and later your baby undergoes critical changes in the few months before ovulation. Through a process called epigenetic changes, which is a change in gene expression a.k.a. genes being turned on and off, the state of health of future parents before conception has long-term effects on baby’s health even in adult life. This means that how you care for your body now directly influences your baby’s future health. Start treating yourself as you would during pregnancy: prioritising nutrition, rest, and overall well-being.
How long before should I start preparing?
The earlier you start, the better. The full process of folliculogenesis, where a primordial follicle develops into a preovulatory follicle ready for ovulation, typically takes about 10-12 months. The process starts to accelerate approximately 90 days before ovulation when the follicle evolves from secondary to pre-antral and starts growing more rapidly. In those 90 days, critical processing of the DNA occurs as well as differentiation in cells within the follicle. This is the window of opportunity to affect egg quality with nutrients, low levels of inflammation, and appropriate hormone levels. If you have less time, don’t worry as any amount of preparation is beneficial.
The four pillars of fertility
To optimise your chances of conception and ensure a healthy pregnancy, it’s essential to focus on the four pillars of fertility: nutrition, lifestyle, toxin management, and supplements.
1. Nutrition
A nutritious, balanced diet is foundational for fertility, especially for women with PCOS. There is a lot of research about diet and fertility, diet and PCOS and less research about diet and fertility in PCOS.
The Mediterranean diet has been shown over and over again to be beneficial for fertility in the general population. It lowers the risk of experiencing difficulty getting pregnant, improves chances of clinical pregnancy and live birth and improves sperm quality amongst others. The Mediterranean diet has also been shown to be beneficial for PCOS especially when combined with a lower carbohydrate consumption.
A 2022 study looked at comparing a low-carbohydrate Mediterranean diet with a low-fat diet. Researchers looked at parameters such as body weight, fasting insulin and blood sugar, insulin resistance, blood lipids and various hormones including luteinizing hormone (LH), follicle-stimulating hormone (FSH), and prolactin (PRL) amongst others. After 12 weeks the Mediterranean diet group had more significant improvements in the menstrual cycle, normalising hormones, weight reduction and improving metabolic parameters.
What about for fertility specifically?
A 2021 systematic review looked at dietary interventions specifically aimed at fertility outcomes such as clinical pregnancy rates, ovulation and menstrual regularity and hormonal markers. 20 studies were included in the analysis. Interestingly, out of those 9 were investigating low-carbohydrate diet, 6 looked at low glycemic index/load diet, four evaluated DASH (Dietary Approaches to Stop Hypertension) diet and 1 trial looked at the Mediterranean diet. Overall these diets were shown to increase rates of clinical pregnancy, ovulation and menstrual regularity, reduce miscarriage rate and improve hormonal parameters. The degree to which diet affected which parameter varied amongst diets. For example both Mediterranean and low-carbohydrate were more-beneficial to pregnancy with improved clinical pregnancy rates and they also had more improvement on menstrual regularity. Por both of those parameters there was a strong correlation between treatment durations with effects becoming much more significant when participant followed the dietary pattern for over 3 months for pregnancy rates and 12 months for menstrual regularity.
2. Lifestyle
Your lifestyle choices significantly impact fertility. Lifestyle includes things like the amount and quality of sleep that we’re getting, the exercise we’re doing, alcohol and caffeine consumption amongst others. One important thing to consider is your stress levels. It’s worth remembering that although sources of stress could be psychological, and they often are in modern life, they also could be physiological such as undereating, over exercising, inflammation, insulin resistance, imbalanced blood sugar, imbalanced gut microbiome and many others.
Let’s see how stress can negatively affect fertility. When your body is stressed it shifts into the fight or flight response meaning the sympathetic nervous system is activated. Your body literally gets prepared to run away from the tiger or to fight it. Certain body functions get prioritised whilst others get slowed down. What gets prioritised is what is needed for your immediate survival - heart rate and blood pressure increase, more oxygen is coming through your lungs, glucose spikes in your bloodstream ready to be used by your muscles. What gets de-prioritised is your digestion, immune system and of course reproductive function.
All these actions are achieved through hormonal activity. It’s primarily adrenaline, noradrenaline and cortisol from adrenal glands. Cortisol is a master hormone in the body meaning it can override the action of other hormones in the name of your survival. Let’s see how it affects reproductive function.
Excessive cortisol can interfere with the pulsatile release of gonadotropin-releasing hormone (GnRH), the hormone released by your brain which controls the menstrual cycle and ovulation, potentially leading to irregular or absent ovulation.
High cortisol levels can also inhibit the release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH), affecting ovarian function and reducing the likelihood of pregnancy
Increased cortisol can lower preovulatory LH peak and estradiol levels, as well as post-ovulatory progesterone and estrogen levels, which can alter endometrial development and reduce the chances of conception
Cortisol dysregulation in PCOS can further exacerbate hyperandrogenism through impact on adrenal DHEA production as well as amplifying insulin resistance, which further stimulates ovarian androgen production
The good news is that there is a lot that we can do to manage our stress levels and whilst some things are outside of our control a lot of things we have control over. Reducing stress is often closely linked with nervous system regulation which primarily involves lifestyle practices. Whatever you resonate with, be it breathing technique, time in nature, yoga, meditation, somatic movement, prayer, just incorporate it as a regular daily practice. Breathing is quite a good one to start because it is so closely linked to the rest-and-digest and fight-or-flight states of our nervous system. Even a few long and deep mindful breaths immediately after you wake up can make a huge difference to your stress levels in the morning. Better yet if you could do at least 10 minutes of breathwork per day.
3. Toxins
Toxins lead to disruption of endocrine (hormonal) health, increased level of inflammation, decreased cell energy production, damage to egg and sperm cells. We’re constantly exposed to various toxins, such as plastics, chemicals in our food and skincare, pesticides, heavy metals, and air pollution. The important thing with toxins is not to get overwhelmed and concentrate on some small manageable baby steps which you can do today to reduce your exposure.
Phthalates
Today we’re going to concentrate on phthalates, which are chemicals found in many household products, cosmetics, and plastics. They are known as plasticizers meaning they increase the shape, flexibility, and durability of plastics, provide structure for products such as hairsprays and nail polish and help scents last longer in the fragranced products. Part of the problem with phthalates is that they are highly soluble in fats and not tightly bound to plastics, they can leach into food products - especially those high in fat, like milk, cheese, and oils.
These chemicals are endocrine disruptors, meaning they can interfere with hormonal balance and potentially worsen symptoms of PCOS. Even in general population phthalates were shown to increase the risk of miscarriage, lower chance of pregnancy in couples undergoing IVF and worsen sperm parameters, although some studies reported limited impact.
A 2024 study found that phthalate exposure in women with PCOS correlated with higher BMI, waist circumference, waist-to-height-ratio, visceral adiposity index, higher fasting glucose, insulin resistance, and dyslipidemia (imbalanced blood lipids). Another study done in 2019 found higher levels of phthalates in the follicular fluid of PCOS patients, potentially impairing granulosa cell function making them produce higher levels of androgens. Those women who had high levels of DEHP (Di(2-ethylhexyl) phthalate) had significantly lower clinical pregnancy rates compared with controls.
How do I reduce exposure?
Avoid using plastic containers for food storage, choose phthalate-free cosmetics and personal care products, and reduce the use of air fresheners and scented household items.. The other sneaky way phthalates get in through an ingredient labeled Fragrance. Since manufactures do not need to fully disclose what is inside “Fragrance” it might as well contain phthalates. Perfumes and colognes are an obvious place to start especially since there are alternatives based on essential oils. Avoiding anything with a strong smell and non-transparent ingredients list might be a good idea. Check product labels for ingredients like DBP (dibutyl phthalate) and DEHP (diethylhexyl phthalate), as these are common phthalates.
4. Supplements
Supplements can bridge nutritional gaps and support specific fertility challenges associated with PCOS. Overall, there is a lot of evidence to show that when chosen correctly for a given situation supplements could be really useful in improving fertility outcomes. Supplements should really be fully personalised as the choice will very much depend on an individual case.
Some supplements however are shown to be particularly beneficial in PCOS. Inositol, particularly myo-inositol, has shown promise in improving insulin sensitivity, regulating menstrual cycles, and supporting ovulation in women with PCOS. These compounds work similarly to insulin in the body, helping to regulate blood sugar levels and reduce androgen excess. Myoinositiol was shown to improve metabolic and hormonal parameters as well ovarian function and the response to assisted-reproductive technology.
What about my partner?
It’s also a good idea for your partner to begin preparation at the same time since sperm takes about 75 days to mature. The process starts in the seminiferous tubules in the testicles under the influence of FSH (follicle-stimulating hormone) where the sperm is produced. Production involves various stages (spermatogonial, spermatocyte and spermatid) and takes around 64 days. In the end of it sperm cells have a tail and hopefully the correct number of chromosomes. After 64 days those sperm cells travel into the epididymis which is a highly-coiled tube attached to the testicles, where they spend further 10-14 days gaining motility and the ability to fertilize an egg.
The specific timeline will vary based on your individual health, age, PCOS management status, and whether you plan to conceive naturally or use assisted reproductive technologies.
I hope you have enjoyed this episode of the fertility series. If you have further questions pop them in to the comments below.
Francesca
Basu, B. R., Chowdhury, O., & Saha, S. K. (2018). Possible Link Between Stress-related Factors and Altered Body Composition in Women with Polycystic Ovarian Syndrome. Journal of human reproductive sciences, 11(1), 10–18. https://doi.org/10.4103/jhrs.JHRS_78_17
Çekici, H., & Akdevelioğlu, Y. (2019). The association between trans fatty acids, infertility and fetal life: a review. Human fertility (Cambridge, England), 22(3), 154–163. https://doi.org/10.1080/14647273.2018.1432078
Chavarro, J. E., Rich-Edwards, J. W., Rosner, B. A., & Willett, W. C. (2008). Use of multivitamins, intake of B vitamins, and risk of ovulatory infertility. Fertility and sterility, 89(3), 668–676. https://doi.org/10.1016/j.fertnstert.2007.03.089
Muffone, A. R. M. C., de Oliveira Lübke, P. D. P., & Rabito, E. I. (2023). Mediterranean diet and infertility: a systematic review with meta-analysis of cohort studies. Nutrition reviews, 81(7), 775–789. https://doi.org/10.1093/nutrit/nuac087
Nazarpour, S., Ramezani Tehrani, F., Simbar, M., & Azizi, F. (2015). Thyroid dysfunction and pregnancy outcomes. Iranian journal of reproductive medicine, 13(7), 387–396. https://pubmed.ncbi.nlm.nih.gov/26494985/
Saadati, N., Haidari, F., Barati, M., Nikbakht, R., Mirmomeni, G., & Rahim, F. (2021). The effect of low glycemic index diet on the reproductive and clinical profile in women with polycystic ovarian syndrome: A systematic review and meta-analysis. Heliyon, 7(11), e08338. https://doi.org/10.1016/j.heliyon.2021.e08338
Yassa, L., Marqusee, E., Fawcett, R., & Alexander, E. K. (2010). Thyroid hormone early adjustment in pregnancy (the THERAPY) trial. The Journal of clinical endocrinology and metabolism, 95(7), 3234–3241. https://doi.org/10.1210/jc.2010-0013
Wang, F., Xie, N., Wu, Y., Zhang, Q., Zhu, Y., Dai, M., Zhou, J., Pan, J., Tang, M., Cheng, Q., Shi, B., Guo, Q., Li, X., Xie, L., Wang, B., Yang, D., Weng, Q., Guo, L., Ye, J., Pan, M., … Qu, F. (2021). Association between circadian rhythm disruption and polycystic ovary syndrome. Fertility and sterility, 115(3), 771–781. https://doi.org/10.1016/j.fertnstert.2020.08.1425