Hello everyone,
This article was quite hard to write and film emotionally. For anyone who wishes to become a mother, the thought of managing to get pregnant and losing it is terrifying. I have added one more episode to the series. So far we have gone through:
Episode 1: PCOS and fertility - how do I know how much time I have left?
Episode 5: The risk of miscarriage
I know numerous women who have gone through miscarriages and then went on to have healthy babies later down the line, or women who needed assistance. The reason why I think it’s important to talk about it is because it normalises it. 90% of miscarriages in the first trimester are down to chromosomal problems - so it’s not your fault if it happens. Many women blame themselves for it, but it’s a natural phenomenon. Of course, we are emotionally intelligent animals, so it’s hard to stay purely in the facts, but understanding the odds is helpful.
Approximately 25% of women experience a miscarriage in their lifetime, so that’s 1 in 4 who will have to go through this unpleasant experience.
I have been very close to two of my friends’ miscarriages and their experience, which, while painful, normalised it. Here are the numbers for women without PCOS and those with PCOS.
❤️ This content is for our paid subscribers. A lot of work and research goes into writing these articles. Consider becoming a paid subscriber to get the most scientifically-backed PCOS information and learn to control your PCOS.
Women without PCOS
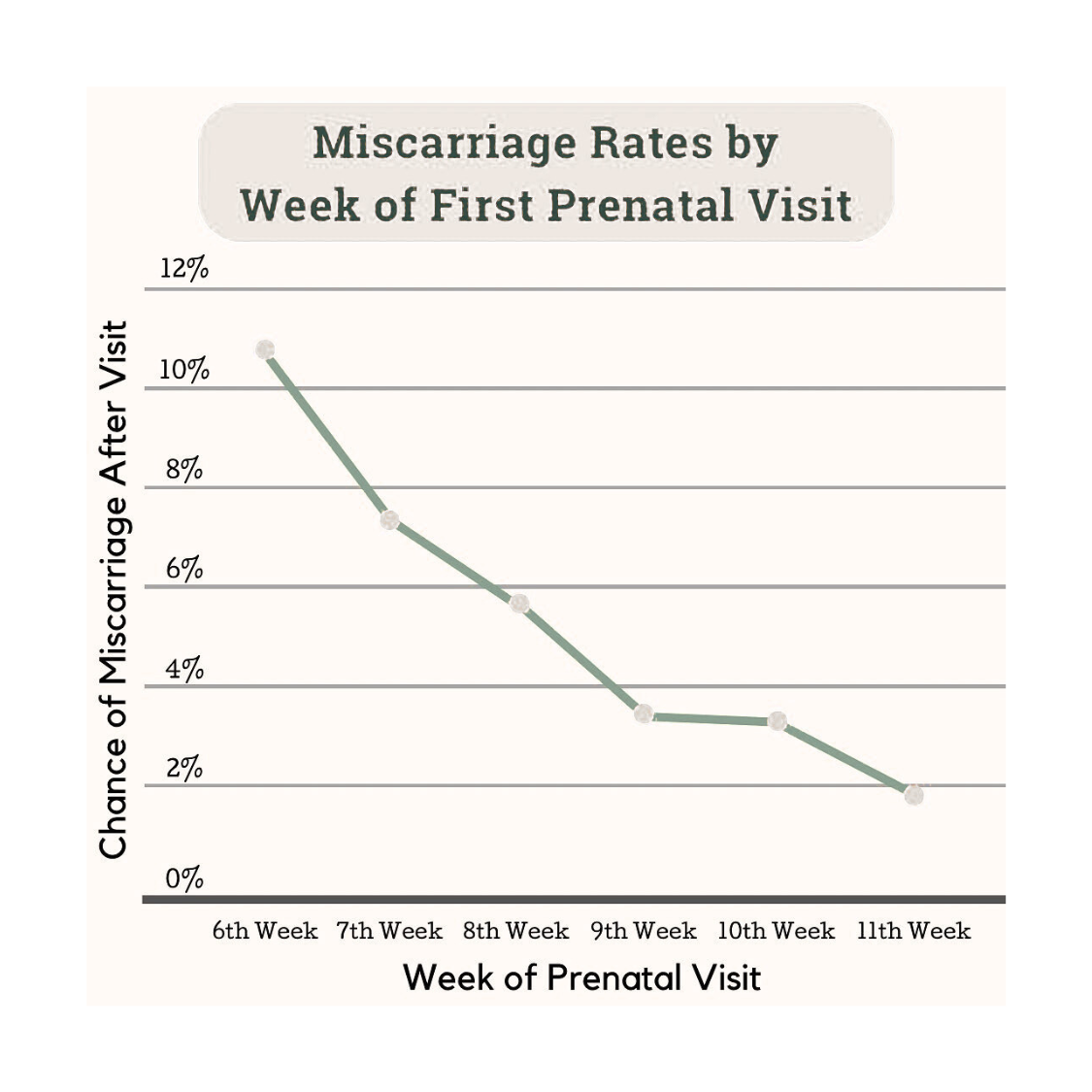
There is a book that provides in-depth details about the data we have on popular pregnancy myths. It’s called Expecting Better by Emily Oster. I can see that she was a very anxious mom-to-be and found a lot of comfort in understanding risk percentages and delving deeply into the data. If you are seen at week 6, and everything looks good, these are the % of pregnancies that are lost afterwards. Starting at 11% in week 6 and going down to 2% in week 11. A very sharp decrease.
Other sources, such as the Tommys, a charity dedicated to pregnancy and babies, report the following numbers: early miscarriages happen to 10-20 in 100 (10 to 20%) of pregnancies. That’s almost 1 in 5. Second-trimester miscarriages happen in 3-4% of pregnancies.
The numbers differ according to the source. As you can imagine, it’s pretty hard to estimate, as some of the miscarriages can go unnoticed when they happen. Some studies even put the risk at week 3 at 30%. The risk of losing your pregnancy goes down as time passes and the little cells become a fetus.
Women with PCOS
It will come as no shock to you that we have a higher chance of miscarriage. With this condition, you can pretty much assume that we have an increased risk of every disease under the sun. It does show the wide range of implications of hormones on our bodies.
A paper on pregnancy in women with PCOS puts our first-trimester miscarriage rate between 30 to 50%. It is pretty challenging to determine, so most of these figures come from studies where some form of assistance was provided. For example, treatment with ovulation-inducing agents such as clomiphene or letrozole is associated with a higher incidence of miscarriage compared to the naturally conceiving population. It is not known the rate of miscarriage for those who conceived naturally. I guess that it depends heavily on how well-controlled your PCOS is.
Why?
1. Increased LH
An increase in LH characterises PCOS. High LH can:
Prematurely trigger oocyte maturation → poorer quality eggs.
Impair corpus luteum function → insufficient progesterone support for early pregnancy - progesterone is needed for the endometrium to develop and be stable where the embryo implants
What can I do?
Before conceiving, it would be ideal to undergo a test to determine your baseline LH levels. Elevated LH is primarily genetic; however, there is evidence that insulin can increase LH secretion - so taking care of your insulin levels MIGHT*** help.
Might*** - with three *** because it’s very hard to prevent miscarriages or be sure of what the issues are - the things that I suggest are in no way saying - if you do this, you won’t have a miscarriage. As we saw at the beginning of this article, most of it’s chromosomal - we are just trying to understand if the percentage increase compared to women without PCOS might be due to PCOS-specific things. I am a control freak - so if there are things that I can try, I will do them even though they might not necessarily have an effect.
2. Elevated androgens
Elevated free/total testosterone ratios were found to be predictive of early pregnancy loss in two different studies.
The authors speculated that high androgen levels antagonise estrogen, which may affect endometrial development and implantation. The endometrium is incredibly important for the embryo to implant and find its cosy home for the next 9 months.
What can I do?
Similarly, testing your testosterone levels beforehand is probably a good idea. It’s all about understanding your baseline and giving yourself 3-12 months prep time. We discuss how to prepare for pregnancy at length in our second episode.
4. Plasminogen activator inhibitor-1 (PAI-1)
High plasminogen activator inhibitor-1(PAI-1) activity is associated with recurrent pregnancy loss in women with unexplained recurrent miscarriages. It has also been found to be significantly higher in women with PCOS. PAI-1 inhibits fibrinolysis - the body’s ability to dissolve clots. Tiny clots can form in the blood vessels that feed the placenta (the organ that supplies the baby with oxygen and nutrients). These clots block the blood flow, so the placenta doesn’t get enough circulation. Without proper blood supply, the placenta can’t support the baby → leading to pregnancy loss.
What can I do?
There is a study which documented improved pregnancy outcomes with metformin in overweight women with PCOS and correlated it to significantly reduced PAI-1 activity levels resulting from treatment. This is an option. Metformin will come up later in the article.
5. Insulin Resistance
You knew this one was coming. This one has multiple implications:
Alters oocyte quality and maturation.
Interferes with glucose uptake in the endometrium → poor energy support for implantation.
Exposure to excess glucose can turn on a “self-destruct switch” ( apoptosis)
Suppresses GLUT4 expression in endometrial cells, reducing glucose transport.
Reduces glycodelin & IGFBP-1 (proteins crucial for implantation and maternal immune tolerance).
What can I do?
Allowing yourself time to adjust your diet before trying to conceive is important. Metformin can also be your friend in these instances, together with Inositol, a low-GI diet and muscle building.
6. Endometrial Dysfunction
Even beyond hormones and insulin resistance, women with PCOS may show:
Reduced β3 integrins → cell adhesion molecules needed for embryo attachment.
Reduced glycodelin → supports placental development and immune modulation
Reduced IGFBP-1 - regulates fetal growth and implantation
Can I do anything to prevent a miscarriage?
There is a retrospective review where 65 women with PCOS who continued metformin during pregnancy had a much lower rate of first-trimester loss (8.8%) compared to 31 women who did not take it (41.9%). Among those with a history of miscarriage, the protective effect was even more substantial (11.1% vs. 58.3%). These findings suggest that metformin use in pregnancy may significantly reduce early pregnancy loss in women with PCOS. There is a current research study ongoing, called the LOCIS Trial, which is due to be published later this year. The LOCI trial will generate robust evidence on whether continuing metformin treatment throughout the 1st trimester can reduce the risk of miscarriage for approximately 1,800 women with PCOS.
I would discuss this with your doctor and consider taking Metformin for a while before you start conceiving and throughout your first trimester.
Lifestyle and weight management are universally recommended and provide broader health and fertility benefits. Looking after our PCOS markers is essential. Supplementation with Vitamin D, Omega-3, and Folate is also very important. A good prenatal multivitamin can help.
If you need specialised support, don’t hesitate to contact me at francesca.abalasei@gmail.com
This concludes our fertility series. I will create a lot more pregnancy content later on. I hope this has offered you a window into what you need to know about this chapter in our lives.
See you next Sunday,
Francesca
Kamalanathan, S., Sahoo, J.P. & Sathyapalan, T., 2013. Pregnancy in polycystic ovary syndrome. Indian Journal of Endocrinology and Metabolism, 17(1), pp.37–43. doi:10.4103/2230-8210.107830.
Jakubowicz, D.J., Iuorno, M.J., Jakubowicz, S., Roberts, K.A. & Nestler, J.E., 2002. Effects of metformin on early pregnancy loss in the polycystic ovary syndrome. Journal of Clinical Endocrinology & Metabolism, 87(2), pp.524–529. doi:10.1210/jcem.87.2.8207.
Tommy’s, Miscarriage statistics. Available at: https://www.tommys.org/baby-loss-support/miscarriage-information-and-support/miscarriage-statistics?gad_source=1&gad_campaignid=22825123180&gbraid=0AAAAAD0uo5RxX0jjNoSUdLB-_NWMLALKe&gclid=Cj0KCQjw2IDFBhDCARIsABDKOJ42HsqaZ2EN3D-imPNSWMPS3e5vJ-yeulVWdoMN8ScD3kXt4lmIu84aAi4gEALw_wcB (Accessed: 17 August 2025).