Menopause: what women with PCOS can expect #108
Does it get worse or better?
Hello everyone,
How is your Sunday going? Are we all ready for Christmas?
Cool fact: did you know the whale family are the only other mammals that experience menopause? All other species reproduce till they die.
That was an interesting segway into today’s topic: what happens at menopause for women with PCOS?
In this newsletter:
What is menopause?
What age do women with PCOS reach menopause: there is some good news: we might reach menopause later.
What happens to our symptoms, including periods, metabolism and mental health?
Do we have worse menopausal symptoms?
Does PCOS go away after menopause?
How can I prepare for it?
The PCOS Newsletter has 30% off for existing subscribers until the end of the year. 2025 will bring incredible insights into PCOS, fertility and meal plans.
First and foremost, let’s quickly define menopause.
Peri-menopause and Menopause
Peri-menopause is the natural decline of our reproductive ability, whilst menopause marks the end and the beginning of a new life stage. As much as it’s seen as a decline and sad moment in women’s lives, I dare to re-frame that into a natural process in our bodies. Menopause is similar to puberty, just another life stage.
Peri-menopause = two to twelve years before your periods stop
Menopause = the life phase that begins one year after your last period.
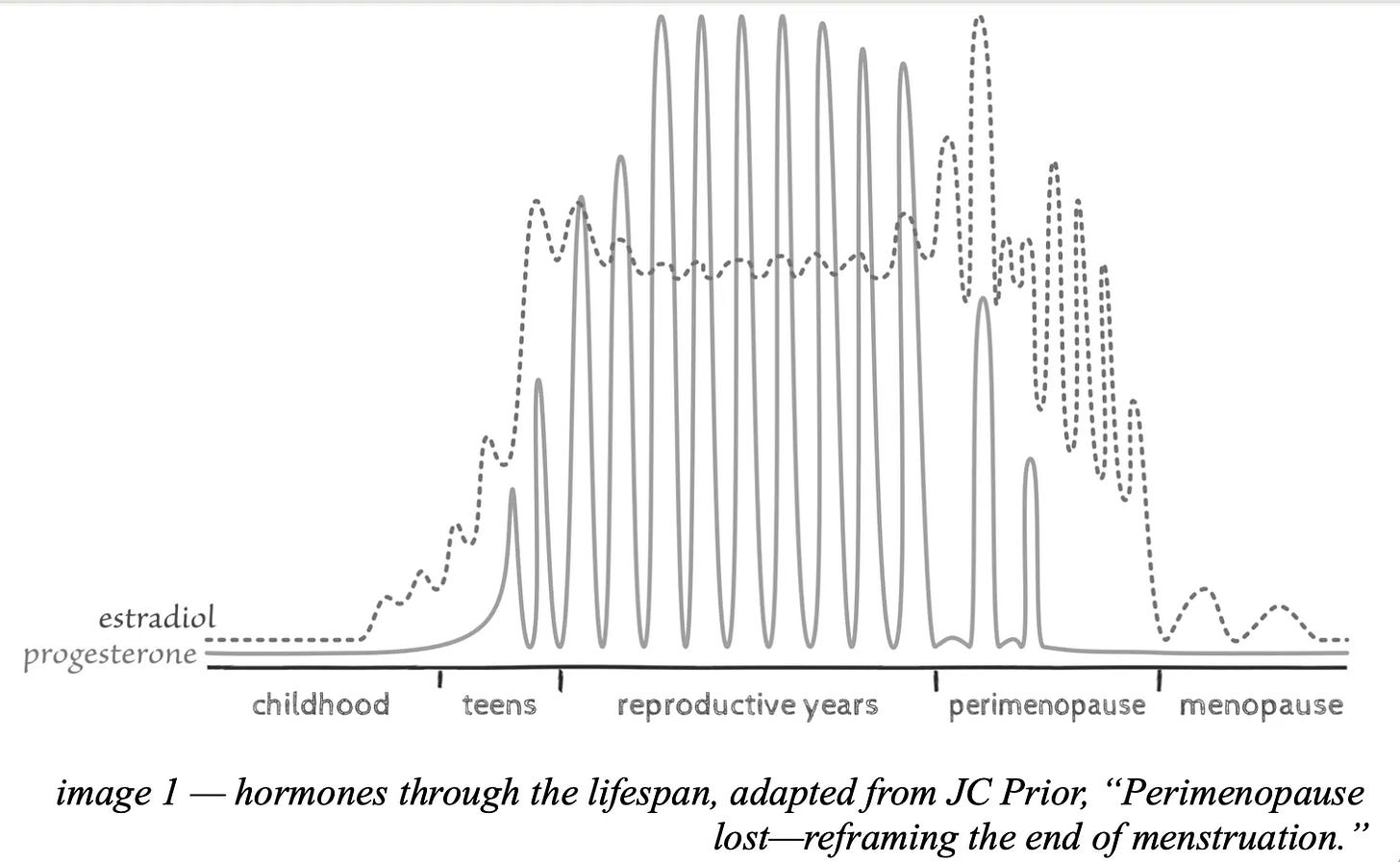
These phases are defined by a shift in our two most important hormones: progesterone and estrogen. These two hormones have their rhythm throughout our whole life 👇🏼.
Progesterone is the first one that we start losing. Due to this loss of progesterone, we can experience symptoms such as anxiety, breast pain, heart palpitations, night sweats, frequent migraines, and heavy periods.
Whilst progesterone declines faster, estrogen doesn’t, so for a while, we start experiencing higher levels of estrogen, which can also cause symptoms such as irritable mood, breast pain, and heavy periods.
This shift in hormones puts women in a vulnerable position. Every window of significant physiological changes, including puberty, pregnancy or menopause, creates an opportunity and/or a risk for new health problems to arise.
I asked Elizabeth Ward, a Registered Dietitian and the author of Menopause Nutrition Substack, what her thoughts on this phase: “I always say that perimenopause is the time to get all your ducks in a row and to establish useful, healthy habits that will help you during and after the menopause.”
The US Study of Women’s Health Across the Nation (SWAN) described perimenopause as “a critical window of opportunity for prevention.”
Why is that?
The shift in hormones changes can contribute to insulin resistance:
Estrogen fluctuations: As estrogen levels become erratic and eventually decline, insulin sensitivity decreases. Estrogen typically helps sensitise cells to insulin, so its reduction can lead to insulin resistance.
Progesterone decline: Lower progesterone levels can destabilize the hypothalamic-pituitary-adrenal (HPA) axis, affecting stress response and blood glucose management
Cortisol increase: The decline in estrogen and progesterone can lead to higher cortisol levels, increasing appetite and cravings for high-sugar foods and contributing to insulin resistance.
This is true not only for women with PCOS but all women. This is why it’s often the case that women gain weight around this time of their lives.
If we already have issues with our insulin resistance, as women with PCOS do, this will be accentuated through this period. Whilst this shift in hormones creates a window of opportunity, I think women with PCOS must take this prevention seriously way before perimenopause comes into question.
Let’s dive deeper into what happens to us when it’s time to hang our reproductive boots (does this analogy sound weird?)
Keep reading with a 7-day free trial
Subscribe to The PCOS Newsletter to keep reading this post and get 7 days of free access to the full post archives.