SHBG - a PCOS protein #87
What is it?
Hello, lovely people
How is your August going? This Friday is my wedding day. I can’t believe it has come around so quickly. Slightly nervous but equally excited.
Today, I wanted to discuss Sex Hormone-Binding Globulin (SHBG). This protein is as vital as LH and FSH in the manifestation of PCOS. For me, it always shows slightly lower in blood test results, and there is a reason why.
Sex Hormone-Binding Globulin (SHBG) is a protein produced in the liver that binds to sex hormones, specifically testosterone. It transports testosterone to the organs where it needs to go. Only 1–2% of testosterone in the circulation is free and active; 65% is bound to SHBG, and the rest is bound to albumin.
As you can tell, there is a very tight control on how much testosterone roams freely in our blood.
SHBG and PCOS
In PCOS, SHBG levels are low. Due to the low levels of SHBG, it causes two issues:
Excess testosterone
This is where the role of this protein is extremely important to us—SHBG regulates how much “free testosterone” is in the blood. When the level of SHBG is lower, more testosterone runs free in the blood, which leads to testosterone overstimulating androgen receptors all over the body.
Let’s take an example:
Our hair cells have androgen receptors. Certain areas of the body, such as the chin or upper lip, are more sensitive to androgen hormones, which is why these areas may have more hair growth. This is also why men have a lot of hair there. In the presence of too much free testosterone, these receptors get stimulated, leading to excess hair growth. If you want a deep dive into how this works, head over to this article.
Of course, too much testosterone in the blood is also what might be stopping our ovulation, leading to irregular periods and fertility issues.
Insulin Resistance
One recent study suggested that SHBG levels below 42 nmol/L should cause closer monitoring for fatty liver and prediabetes. They observed a 50% probability of insulin resistance at an SHBG concentration of 41.1 nmol/L.
Higher levels of insulin seem to inhibit the production of SHBG in the liver, leaving us with excess testosterone. Excess testosterone can directly impair insulin signalling pathways, leading to decreased insulin sensitivity. In addition, elevated testosterone levels are associated with increased visceral fat, which is the fat stored around the organs, which worsens insulin resistance. It’s a bit of a vicious cycle.
Why is it low in women with PCOS?
Excess insulin
Insulin reduces circulating SHBG levels by reducing the production of SHBG in the liver, which increases the level of testosterone in the blood. This elevated testosterone further aggravates insulin resistance, ultimately creating a vicious circle.
Excess weight
Low plasma SHBG levels are related to obesity, especially abdominal obesity. Studies have shown that body weight, particularly the ratio between fat tissue and lean muscle, is among the most important determinants of SHBG levels.
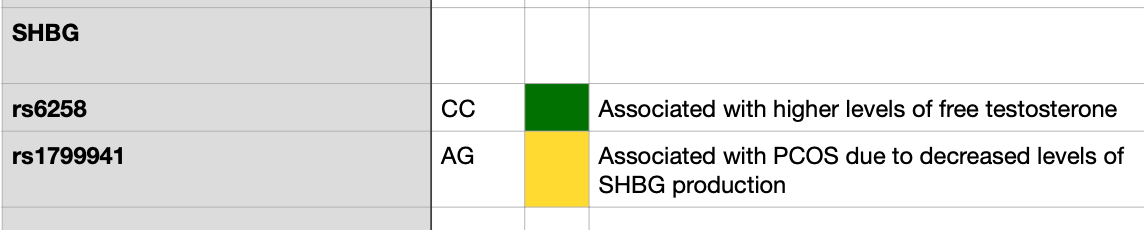
SHBG gene variation
Certain gene variations have been linked to low levels of SHBG in women with PCOS. Three variations of the SHBG gene are also linked to the risk of developing type 2 DM. This suggests that SHBG may have a role in the development of type 2 DM through the development of insulin resistance.
We will be testing the SHBG gene in our Genetics-based Programme. A 16-week programme designed to help you take control over your PCOS once and for all. You can learn more and secure your spot here: www.pcos-clinic.com.
I have one of the PCOS variations 👇🏼:
How can you increase SHBG?
Decreasing insulin levels
One of the most important things is to decrease insulin levels. This means changing your diet to ensure that you are not regularly spiking your glucose levels, weight loss, and eating lower-glycemic foods overall.
Vitamin D supplementation
We have discussed Vitamin D deficiency at length here. Approximately 67–85% of PCOS women show vitamin D deficiency. That is a crazy statistic. A study looking at a high dose of Vitamin D daily for 12 weeks shows a significant increase in SHBG. I wouldn’t be surprised if those people had a variation in the Vit D gene and, as a result, needed a bigger dose.
Isoflavones
A study found a significant diet-gene interaction between isoflavones (phytoestrogens found in soy products) and the D327N variation of the SHBG gene. In women carrying the D327N variant, isoflavones were shown to stimulate SHBG levels.
A diet low in fat and high in fibre
A lower fat (>10% of calories per day) and high fibre were associated with increased SHBG. Now imagine being on a keto diet with this variation…
Have you had your SHBG levels tested for your PCOS?
See you next week for a personal update on my wedding!
Francesca
Jamilian, M., Foroozanfard, F., Rahmani, E., Talebi, M., Bahmani, F., & Asemi, Z. (2017). Effect of two different doses of vitamin D supplementation on metabolic profiles of insulin-resistant patients with polycystic ovary syndrome. Nutrients, 9(12), 1280. https://doi.org/10.3390/nu9121280
Lin, J., Wu, W., Weng, Y., Lan, Y., Wen, Y., Lai, S., Fu, X., Kuang, J., Guan, H., & Chen, H. (2024). Correlation between serum sex hormone-binding globulin levels and nutrition indicators and malnutrition exposure risk in men and postmenopausal women with type 2 diabetes. BMC Endocrine Disorders, 24(1). https://doi.org/10.1186/s12902-024-01653-x
Qu, X., & Donnelly, R. (2020). Sex hormone-binding globulin (SHBG) as an early biomarker and therapeutic target in polycystic ovary syndrome. International Journal of Molecular Sciences, 21(21), 8191. https://doi.org/10.3390/ijms21218191
Unluhizarci, K., Karaca, Z., & Kelestimur, F. (2021). Role of insulin and insulin resistance in androgen excess disorders. World Journal of Diabetes, 12(5), 616–629. https://doi.org/10.4239/wjd.v12.i5.616
Wallace, I. R., McKinley, M. C., Bell, P. M., & Hunter, S. J. (2013). Sex hormone binding globulin and insulin resistance. Clinical Endocrinology, 78(3), 321–329. https://doi.org/10.1111/cen.12086
Xing, C., Zhang, J., Zhao, H., & He, B. (2022). Effect of sex hormone-binding globulin on polycystic ovary syndrome: Mechanisms, manifestations, genetics, and treatment. International Journal of Women’s Health, 14, 91–105. https://doi.org/10.2147/ijwh.s344542
Xita, N., & Tsatsoulis, A. (2010). Genetic variants of sex hormone-binding globulin and their biological consequences. Molecular and Cellular Endocrinology, 316(1), 60–65. https://doi.org/10.1016/j.mce.2009.08.025
Disclaimer: We are all unique in our ways, so this information is for educational purposes only. In my communications, I summarise research data and bring my experience. This shouldn’t be viewed as medical advice at any point. Please consult your healthcare provider further about your health needs