PCOS and Endometriosis #75
Is PCOS linked to Endometriosis?
Hello everyone,
I am writing this as I am off to my hen do (bachelorette party). I am looking forward to a weekend with my dearest and closest friend. However, I couldn’t leave you without a newsletter this week.
Let’s dive into another condition related to hormonal imbalance: Endometriosis.
This week’s question:
Is PCOS linked to Endometriosis?
Endometriosis
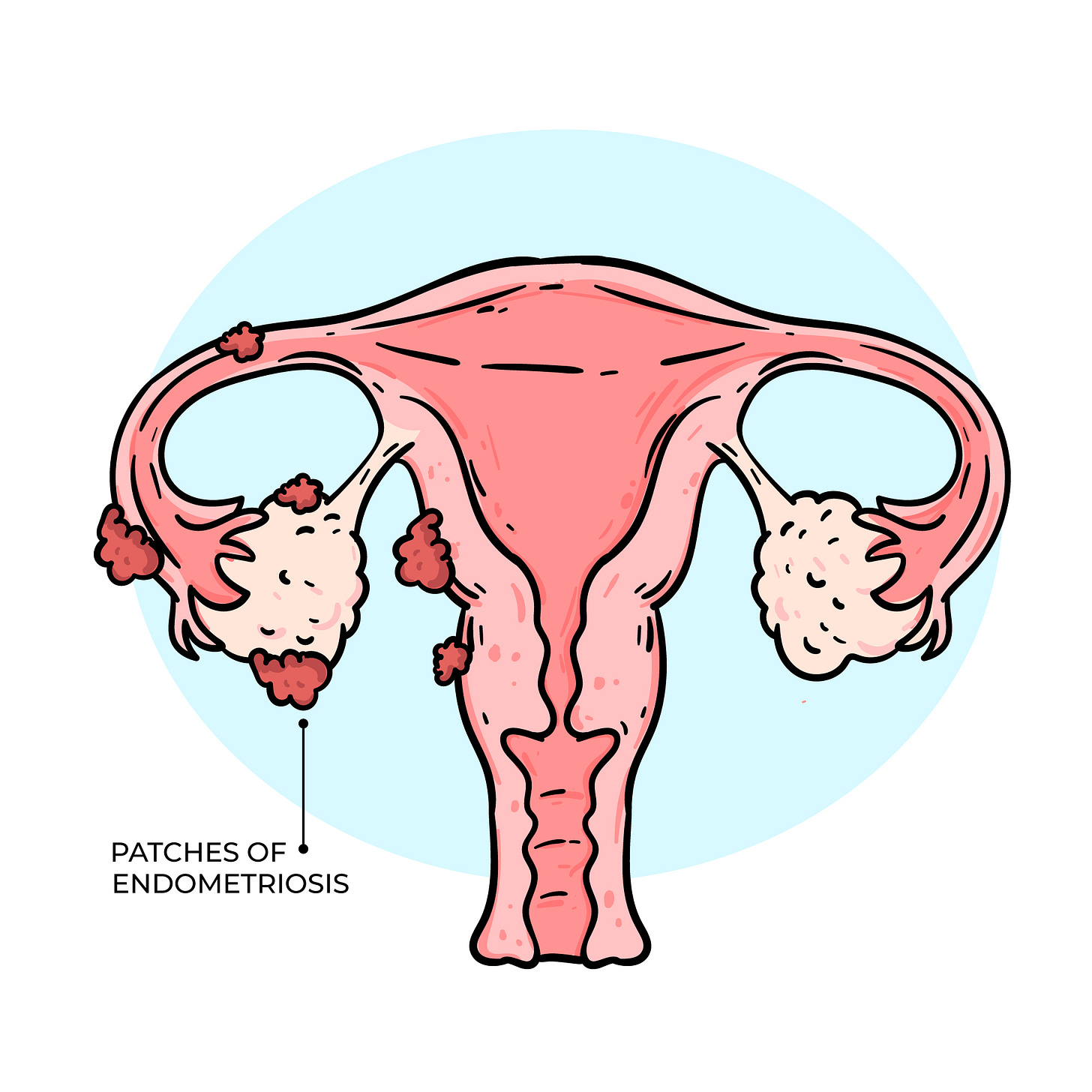
Endometriosis is a condition where tissue similar to the lining of the uterus grows in other parts of the body. This includes the fallopian tubes, lining of the pelvic cavity, ovaries, outside surface of the uteru and rarely around org A very odd quark of nature. Its main symptoms are chronic pelvic pain and infertility. It is thought to affect 6%–10% of women of reproductive age. However, diagnosis is only confirmed when surgery is performed, and this tissue is found. I don’t even want to imagine how many women suffer in pain, not knowing that they have this condition. Research is trying to figure out better ways of diagnosing it, but so far, there haven’t been any that worked.
Just a reminder, this tissue is your period. The lining of the uterus grows under the influence of estrogen and sheds during your period. However, when it grows in a place where it shouldn’t, it responds to the same hormone but can’t shed. It leads to inflammation, scarring and painful cysts. It can also lead to a buildup of fibrous tissues between reproductive organs that causes them to “stick” together.
The main symptoms of endometriosis are painful periods, pain during sex, heavy periods, irregular periods, and pain when passing bowels or urination. Other symptoms include extreme tiredness, nausea, depression and frequent infections such as thrush (candida).
Surprisingly, it seems to occur in other species that menstruate, including higher primates (humans, macaques, and baboons) and some monkeys (cynomolgus).
What causes it?
Endometriosis is reported to “run in families,” with results from twin studies suggesting heritability may be as high as 50%.
The cause of it is not fully understood. The more I work in this field, the more I realise the large amount of diseases that have no clear cause. There are some theories:
Retrograde menstruation: This theory suggests that when you have a period, some of the endometrium (womb lining) flows backwards through the fallopian tubes and into the abdomen. This tissue then implants itself on organs in the pelvis and grows. It has been suggested that most women experience some form of retrograde menstruation, but their bodies can clear this tissue, and it does not deposit on the organs. This theory does not explain why endometriosis has developed in some women after hysterectomy or why, in rare cases, endometriosis has been discovered in some men when they have been exposed to oestrogen through drug treatments.
Lymphatic or circulatory spread: This theory states that endometriosis tissue particles somehow travel around the body through the lymphatic system or the bloodstream. This could explain why it has been found in areas such as the eyes and brain.
Environmental causes – such as dioxin exposure: The theory is that certain toxins in our environment, such as dioxin, can affect the body, the immune system and the reproductive system and cause endometriosis. Research studies have shown that when animals were exposed to high levels of dioxin, they developed endometriosis. This theory has not yet been proven for humans.
Metaplasia is the process where one type of cell changes or morphs into a different kind of cell. Metaplasia usually occurs in response to inflammation and enables cells to adapt to their surroundings to better adapt to their environment. In the case of endometriosis, metaplasia would explain how the endometriosis cells appear spontaneously inside the body – and how they appear in areas such as the lungs and skin. It would also explain the appearance of endometriosis cells in women with no womb – or in men who have taken hormone treatments.
Endometriosis and PCOS
Some believe it to be somehow the same condition but on opposite ends. In endometriosis, the levels of LH, testosterone, and anti-Müllerian hormone (AMH) decrease, whereas the levels of follicle-stimulating hormone (FSH), sex hormone-binding globulin (SHBG), and oxytocin increase. On the other hand, we have increased LH, AMH, and androgens levels while decreased levels of FSH, SHBG, and oxytocin have been detected. The hormone that drives these conditions are the same but on opposite ends.
There is a theory that suggests that PCOS develop in a mother's womb due to excess testosterone, whereas endometriosis can develop when testosterone is decreased. This can be seen physically:
Anogenital distance (AGD) is defined as the distance between the anus and external genitalia, which is measured in men from the base of the scrotum to the anus and women from the end of the vagina to the anus.
Another difference between men and women is the ratio of the 2nd to the 4th finger length (2D:4D), which is lower in men than women. The difference in AGD and 2D:4D indices in men and women results from the exposure of embryos of each sex to different levels of testosterone during prenatal development.
In PCOS, these two parameters show values close to the male pattern, while in endometriosis, the lowest values of the female pattern indicate the role of testosterone levels in the development of reproductive organs during intrauterine growth of the female fetus and the probability of occurrence of these two diseases after puberty.
These are not reliant ways to diagnose or judge a condition but very interesting differences between men and women when exposed to testosterone.
However, these two conditions can co-exist, which questions the above theory. A study looking at women who underwent surgery to remove endometrial tissue found that 5% had both PCOS and Endometriosis. The sample size was small: 473 women.
Where in the world there is more endometriosis vs PCOS?
Epidemiological studies show that the prevalence rates of endometriosis are higher in Asian and European women in comparison with African populations. In contrast, the incidence of PCOS among Asian and European is lower than African women. Measurement of serum testosterone during pregnancy in these three populations of women confirmed the above hypothesis; accordingly, higher level of testosterone in African pregnant women increases the risk of PCOS and reduces the risk of endometriosis in their daughters, and lower level of testosterone in Asian and European women increases the risk of endometriosis and reduces the risk of PCOS in their daughters.
I hope you have deepened your understanding of this condition. Discussing these adicent conditions is important as it may allow us to recognise them in other women and encourage them to get help.
Have a lovely Sunday,
Francesca
www.pcos-clinic.com
If you are ready to invest in managing your PCOS, you might consider working with me individually. You can book a discovery call here.
Crespi, B. (2021). Variation among human populations in endometriosis and PCOS A test of the inverse comorbidity model. Evolution, Medicine, and Public Health, 9(1), 295–310. https://doi.org/10.1093/emph/eoab029
Endometriosis. (n.d.). Hopkinsmedicine.org. Retrieved 5 June 2024, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/endometriosis
Sadeghi, M. R. (2022). Polycystic ovarian syndrome and endometriosis as two evil extremes of health continuum. Journal of Reproduction & Infertility, 23(1), 1. https://doi.org/10.18502/jri.v23i1.8445
Saunders, P. T. K., & Horne, A. W. (2021). Endometriosis: Etiology, pathobiology, and therapeutic prospects. Cell, 184(11), 2807–2824. https://doi.org/10.1016/j.cell.2021.04.041
Schliep, K. C., Ghabayen, L., Shaaban, M., Hughes, F. R., Pollack, A. Z., Stanford, J. B., Brady, K. A., Kiser, A., & Peterson, C. M. (2023). Examining the co-occurrence of endometriosis and polycystic ovarian syndrome. AJOG Global Reports, 3(3), 100259. https://doi.org/10.1016/j.xagr.2023.100259
Disclaimer: We are all unique in our ways, so this information is for educational purposes only. In my communications, I summarise research data and bring my experience. This shouldn’t be viewed as medical advice at any point. Please further consult your healthcare provider about your health needs.