Are you getting enough folate? The MTHFR gene and PCOS
MTHFR Gene
Hello lovely people,
How are you doing this week?
Today, let’s discuss a topic that arose in a conversation with a friend this weekend: folate and the prevalence of folate deficiency. My friend has a genetic mutation on her folate genes, let’s dive into it and see if you might have it.
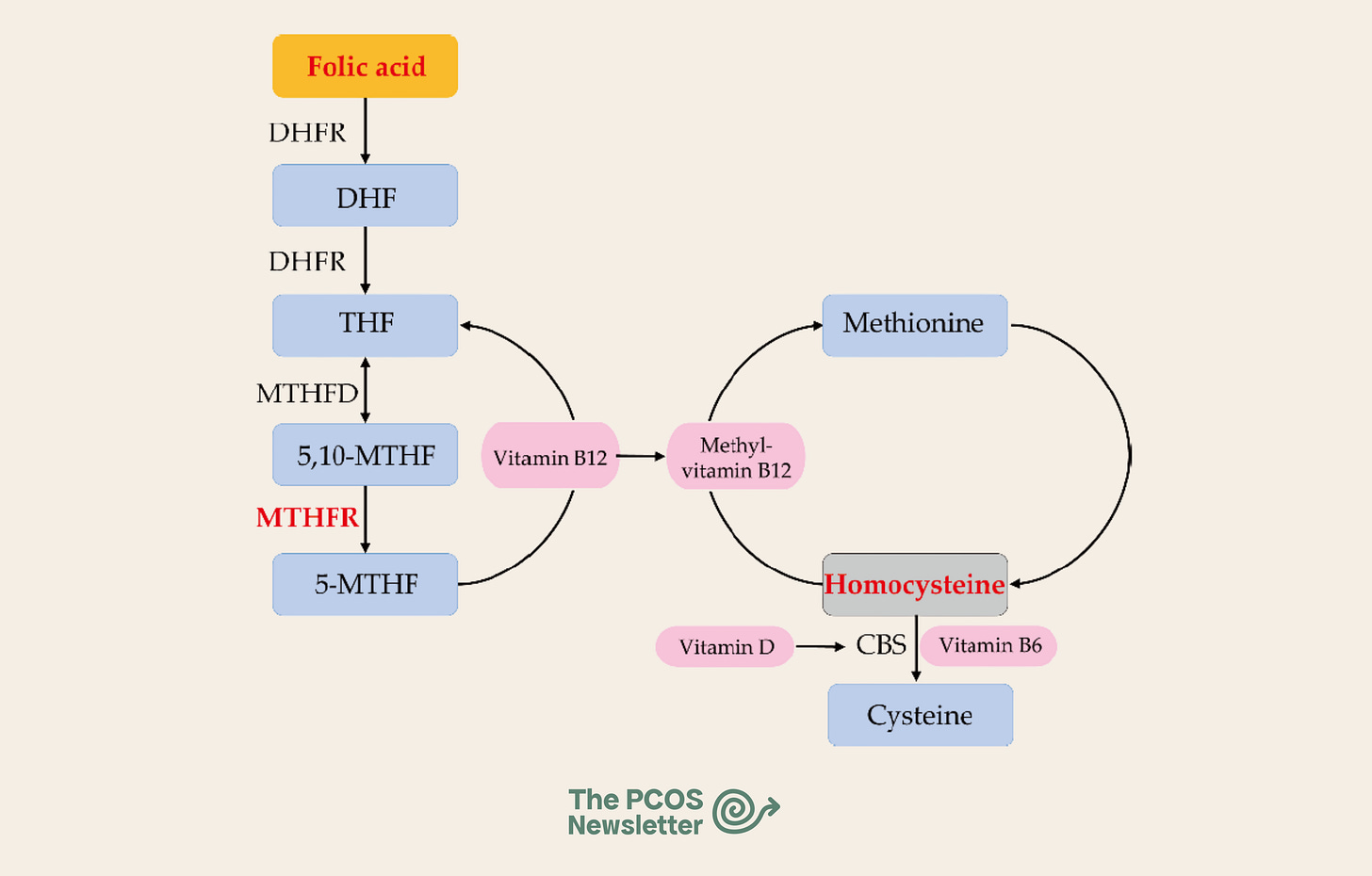
First and foremost, let’s go through why folate is so essential for your health. Besides contributing to the making of DNA and RNA (which is why it’s so important in early pregnancy) and helping red blood cells be produced, folate keeps in check an interesting protein called homocysteine.
Homocysteine is a natural amino acid that we obtain as part of the process of breaking down another amino acid called methionine, which is found in protein in our diet. If its levels get too high, it can increase your risk of heart disease, stroke, pregnancy complications, and even cognitive issues. To break it down, you need three important nutrients: folate, B12 and B6.
Multiple studies and meta-analyses have demonstrated that homocysteine concentrations are significantly increased in women with PCOS, regardless of body mass index (BMI), insulin resistance, or androgen levels, which is why we discuss it today. It can interfere with our ovulation, CVD risk and pregnancy outcomes.
Ok, but why is folate a problem these days?
On the one hand, there's a lack of folate in the diet, but that’s a simple fix. The more pressing problem is genetic variations in the MTHFR gene.
What is MTHFR?
MTHFR stands for methylenetetrahydrofolate reductase—a bit of a mouthful. This gene gives your body instructions to make an enzyme that helps process folate (vitamin B9) and convert it into its active form. The number of processes our nutrients undergo in the body is crazy and fascinating.
This gene is subject to some annoying mutations. These are just small changes in the gene’s code, and the two most common are called C677T and A1298C. You inherit one copy of the MTHFR gene from each parent, so you could have:
No mutations (the “standard” version)
One mutation (heterozygous)
Two mutations (homozygous)
Having one mutation is pretty standard and usually doesn’t cause any issues. Having two C677T mutations can reduce the enzyme’s activity, which may affect how your body processes folate and homocysteine.
60–70% of people have at least one of these two common MTHFR variants. In Europe, about 13.5% carry two C677T variants. In America, 5–14% and 20% in some Latino and Hispanic populations. The people who are the luckiest in these regards are those of African descent, which is found in about 1% of the population.
Multiple studies and meta-analyses have found that the frequency of MTHFR mutations (especially the C677T and A1298C variants) is significantly higher in women with PCOS than in control groups without PCOS. Can we get a f*** break?
I genuinely hope that these pieces of content are helping you manage this condition better and learn this thing we need to live with. If you find it valuable, consider becoming a paid subscriber to have access to all the tools you need to manage your condition and learn in an evidence-based manner.
Should you get tested?
Testing for MTHFR mutations is available, but it’s not routinely recommended for everyone. I have done mind because I am obsessed with everything science and I can order it for you through my nutrigenomics partner if you’d like. Here is my result:
What can you do if you have an MTHFR mutation?
If you do have a mutation, don’t worry—there are practical steps you can take:
Eat plenty of leafy greens and foods rich in natural folate (see examples below)
Consider a methylated folate supplement (not just regular folic acid) - this is the already processed folate so it jumps one step in the process of activation
Make sure you’re getting enough B vitamins (B6, B12).
Manage other risk factors for heart disease: don’t smoke, keep active, and eat a balanced diet.
Foods high in folate
Lentils
Edamame (green soybeans)
Chickpeas
Kidney beans
Black-eyed peas
Asparagus
Spinach
Broccoli
Brussels sprouts
Beets
Avocado
Oranges and orange juice
Sunflower seeds
Liver (beef, chicken, or lamb—avoid during pregnancy)
Peanuts
What’s the difference between folate and folic acid?
Folate and folic acid are both forms of vitamin B9, but they are not the same:
Folate is the natural form of vitamin B9 found in foods like leafy greens, beans, and citrus fruits. Your body absorbs and uses it directly from these foods but it also needs to go through the MTHFR gene for processing.
Folic acid is the synthetic form of vitamin B9, used in supplements and added to fortified foods (like breakfast cereals and bread). It needs to be converted by your body—mainly in the liver—before it becomes active.
What symptoms should I look for?
Most people with an MTHFR mutation have no symptoms at all. If symptoms do appear, they’re usually related to the conditions above, not the gene itself. Some people report:
Fatigue or low energy
Mood swings, anxiety, or depression
Migraines
Pregnancy complications
Unexplained blood clots
But again, these are common symptoms with many possible causes, so don’t panic if you see yourself on this list!
MTHFR is just one piece of your genetic puzzle. For most people, it’s not something to lose sleep over. If you’re feeling overwhelmed by all the genetic talk, remember: your genes are not your destiny. Lifestyle, nutrition, and self-care are just as important, if not more so.
Take care of yourself, and see you next Sunday!
Francesca
Fu, L., Dai, L., Li, X., Zhang, K. & Bai, Y. (2013) 'Association of methylenetetrahydrofolate reductase gene C677T polymorphism with polycystic ovary syndrome risk: a systematic review and meta-analysis update', Maturitas, 76(2), pp. 172–178.
Kondapaneni, V., Rao, S., & Kondapaneni, S. (2020) 'Significance of Homocysteine Levels in the Management of Polycystic Ovarian Syndrome: A Literature Review', Cureus, 12(10), e11123.
Meng, Y., Lin, J., Chen, Y., Xu, T., & Wang, C. (2016) 'Association between High Serum Homocysteine Levels and Polycystic Ovary Syndrome: A Meta-Analysis', PLoS ONE, 11(6), e0157389.
Salehpour, S., Manzor-al-ajdad, O., Neisani Samani, E., & Abadi, A. (2011) 'Evaluation of Homocysteine Levels in Patients with Polycystic Ovarian Syndrome', International Journal of Fertility & Sterility, 5(2), pp. 87–90.
Szafarowska, M., Dziech, E., & Jerzak, M. (2018) 'The Relationship between Homocysteine Levels, MTHFR C677T and A1298C Polymorphisms and Recurrent Pregnancy Loss in Women with and without Polycystic Ovary Syndrome', International Journal of Molecular Sciences, 19(10), 3246.
Li, Y., et al. (2020) 'Significant association between methylenetetrahydrofolate reductase C677T polymorphism and polycystic ovary syndrome: a meta-analysis', Medicine, 99(4), e18816.
ECE2023 (2023) 'Prevalence of MTHFR polymorphisms and metabolic outcomes in women with PCOS', Endocrine Abstracts, 90, EP1157.
McNulty, H., et al. (2019) 'Ethnogeographic prevalence and implications of the 677C>T and 1298A>C MTHFR polymorphisms in US primary care populations', Future Science OA, 5(6), FSO390.
Martínez de Villarreal, L., et al. (2016) 'Heterogenous Distribution of MTHFR Gene Variants among Mestizos and Diverse Amerindian Groups from Mexico', PLoS ONE, 11(9), e0163248.
Zhi, X., et al. (2016) 'Geographical and Ethnic Distributions of the MTHFR C677T Polymorphism', PLoS ONE, 11(4), e0154532.
Maleedhu, P., et al. (2014) 'Status of Homocysteine in Polycystic Ovary Syndrome', Journal of Clinical and Diagnostic Research, 8(2), pp. 31–33.
Glueck, C.J., et al. (2002) 'Polycystic ovarian syndrome and thrombophilia', Human Reproduction, 17(2), pp. 314–319.


Also called the mother *ucker mutation! 🤣 one of my friends had this and it was only caught by a naturopath